In my Health, Technology, and Engineering (HTE) class, we had another speaker, Dr. Brian Prestwich, come in and talk about the $3 trillion U.S. healthcare system.
When the pricing model for software changed from an upfront license fee to a pay-as-you-go subscription used for cloud-based services, it revolutionized the technology industry. Similarly, the healthcare pricing model is changing from volume-based care to value-based care and it is revolutionizing the healthcare industry.
This change has been pushed forward largely due to Obamacare, more accurately called the Affordable Care Act. It is a law that challenges healthcare providers (hospitals, physician clinics, etc) to focus on the value a patient is receiving. Prior to this, doctors would be paid per procedure – a fee for service. Now, doctors are paid for positive patient outcomes – a fee for value.
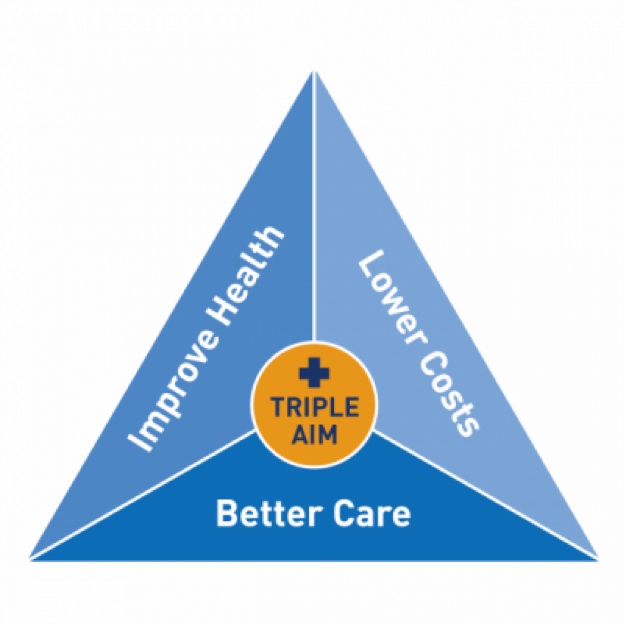
The framework that guides this transformation is the Triple Aim, defined by IHI. The 3 aspects of values-based outcomes are:
Improving the patient experience and quality of care (did patient actually get better and did they feel like they did?)
- Improving population health (how can we treat similar patients in the community and chronic conditions?)
- Minimizing cost (how cost-effective was the treatment/care?)
The actors involved are:
- Patients – those being treated, the customer
- Providers – hospitals, clinics, physicians who give services to patients and try to meet the Triple Aim
- Payers – insurance companies, HMOs, the government health exchanges, etc who reimburse, or pay, the providers for the treatments and now are moving to a fee for value payment system
Though it brings upheaval and controversy, healthcare reform is heading in the right direction. By focusing on a fee for value and evidence-based medicine that determines how effective treatments actually are, the U.S. healthcare system is on a path towards (hopefully) better healthcare.
Published on September 11th, 2016Last updated on April 1st, 2021
